Renin Angiotensin System Inhibitors Versus Other Types Of
Di: Ava
Arterial hypertension is a common worldwide condition characterized by a progression toward high-risk diseases such as ischemic heart disease, heart failure, stroke, and chronic kidney disease. Arterial hypertension can be triggered by many factors, and molecules of the renin–angiotensin–aldosterone system (RAAS) play important roles in the control of blood Background: The effect of angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs) on mortality was preliminarily explored through the comparison of ACEIs/ARBs with non-ACEIs/ARBs in patients with Abstract Aims: We aim to perform a systematic review and meta-analysis examining randomized controlled trials assessing the efficacy and safety of sacubitril/valsartan in patients on renal outcomes, in comparison with the renin
Renin–angiotensin system
Conversely, drug-induced regression of LVM predicts improved outcomes. Previous studies have favored renin-angiotensin system inhibitors (RASIs) over other antihypertensives for reducing LVM but ignored differences among thiazide-type diuretics. Study selection: Randomised clinical trials of antihypertensive therapy (angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), α blockers, β blockers, calcium channel blockers, diuretics, and their combinations) in patients with diabetes with a follow-up of at least 12 months, reporting all cause mortality, requirement for
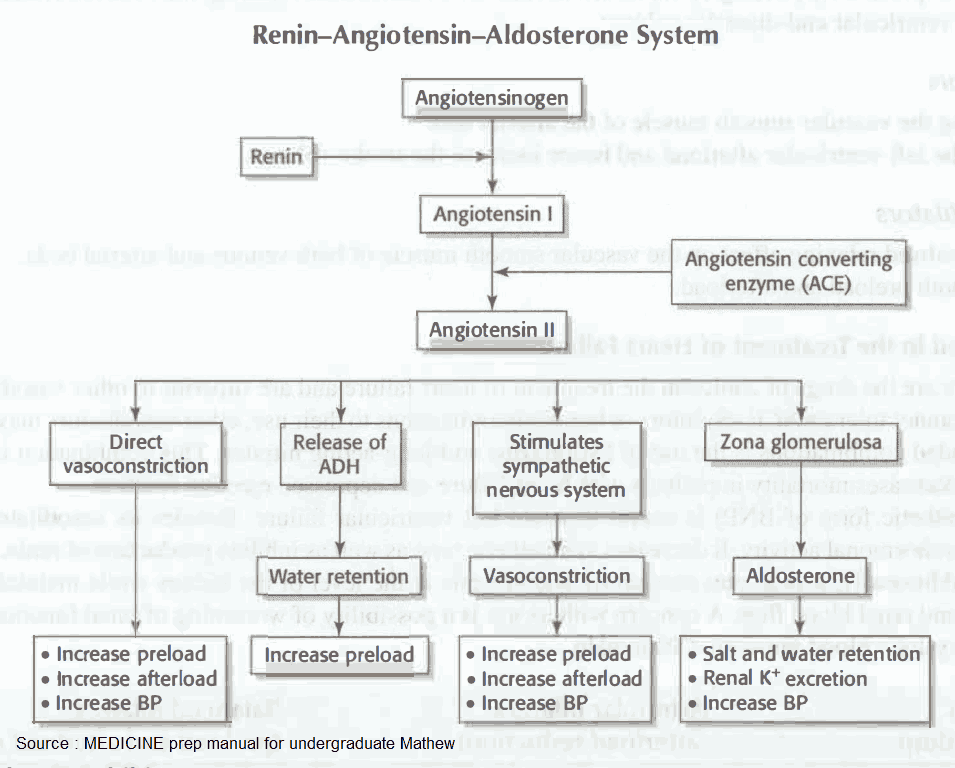
Abstract Background: Chronic treatment of hypertension or heart failure very often includes an angiotensin-converting enzyme inhibitors (ACE-Is) or angiotensin receptor blockers (ARBs) as renin-angiotensin system inhibitors (RASi) treatments. To stop or not to stop these medications before major surgery remains an unresolved issue. The renin-angiotensin system plays critical roles in maintaining normal cardiovascular functions and contributes to a spectrum of cardiovascular diseases. Classically, the renin-angiotensin system is composed of AGT (angiotensinogen), renin, angiotensin-converting enzyme (ACE), Ang II (angiotensin II), and 2 Ang II receptors (AT1 and AT2 receptors). 1, 2 AGT, a protein with 452 Introduction National and international guidelines endorse the view that inhibition of the renin-angiotensin system with angiotensin-converting-enzyme (ACE) inhibitors should be first-line antihypertensive therapy in patients with diabetic and non-diabetic nephropathy.
The classical view of the renin-angiotensin system (RAS) is that of the circulating hormone pathway involved in salt and water homeostasis and blood pressure regulation. It is also involved in the pathogenesis of cardiac and renal disorders. This First-line drugs inhibiting the renin angiotensin system versus other first-line antihypertensive drug classes for hypertension. Cochrane Database of Systematic Reviews 2018, Issue 11.
Renin-angiotensin-aldosterone system inhibitors constitute an important drug class for the treatment of cardiovascular disease. They are 1st-line antihypertensive agents, in addition to being used in the treatment of MI, heart failure, diabetic nephropathy, and stroke. Renin-angiotensin-aldosterone system inhibitors include ACEis, ARBs, direct renin inhibitors (DRIs), Effect of Neprilysin Inhibition on Renal Function in Patients with Type 2 Diabetes and Chronic Heart Failure Who Are Receiving Target Doses of Inhibitors of the Renin-Angiotensin System: a Secondary Analysis of the PARADIGM-HF Trial.
Renin-angiotensin system (RAS) inhibitors reduce risk of kidney failure in patients with chronic kidney disease, but worsen kidney function in heart failure patients, especially in those with chronic kidney disease. Less is known about risk of kidney failure in heart failure patients receiving RAS inhibitors. Abstract Background: It is unknown whether stopping renin-angiotensin system (RAS) inhibitor therapy in patients with advanced CKD affects outcomes. Methods: We studied patients referred to nephrologist care, listed on the Swedish Renal Registry during 2007-2017, who developed advanced CKD (eGFR<30 ml/min per 1.73 m 2) while on RAS inhibitor
The angiotensin receptor–neprilysin inhibitor sacubitril–valsartan simultaneously blocks the renin–angiotensin system and inhibits the breakdown of several vasoactive peptides. 7 In patients Abstract First-line renin-angiotensin system (RAS) inhibitors are recommended for diabetic patients because of their potential nephron-protective properties. For hypertensive patients with type 2 diabetes mellitus, little is known about first-line RAS inhibitors vs. other first-line antihypertensive agents in terms of cardiovascular The optimal management of renin-angiotensin system inhibitors (RASIs) before noncardiac surgery remains unclear. Continuing RASIs may increase intraop
Renin-Angiotensin-Aldosterone System Inhibitors
The renin-angiotensin system is an enzymatic cascade that starts with the cleavage of angiotensinogen by renin to form the inactive decapeptide angiotensin I. Thereafter, angiotensin I is converted by ACE to form angiotensin II. Although there are other angiotensin peptides with biological effects, angiotensin II is the major end product of the system. However,
The renin-angiotensin-aldosterone system (RAAS) regulates the body’s hemodynamic equilibrium, circulating volume, and electrolyte balance, and is a key therapeutic target in hypertension, the world’s leading cause of premature mortality. Fig 3 Forest plot showing effect of renin angiotensin system inhibitors (RASi) versus placebo or active controls on cardiovascular mortality in patients with stable coronary artery disease without heart failure. The current guidelines regarding the continuation or discontinuation of renin-angiotensin-aldosterone system inhibitors (RAAS) inhibitors before noncardiac surgery are conflicting. This meta-analysis aims to evaluate whether continuing or withholding RAAS inhibitors before noncardiac surgery influences perioperative mortality and complications.
The renin-angiotensin-aldosterone system (RAAS) is a critical regulator of blood volume, electrolyte balance, and systemic vascular resistance. While the baroreceptor reflex responds in the short-term to decreased arterial pressure, the RAAS is responsible for acute and chronic alterations. The classical understanding of RAAS is that it comprises 3 significant When compared to placebo, mineralocorticoid receptor antagonists (MRAs) significantly reduced the risk of all-cause mortality and cardiovascular mortality, while none of other RAAS modulators significantly lowered the risk of all-cause or cardiovascular mortality. MRAs were the only renin-angiotensin-aldosterone modulators with a survival benefit in adults
The therapeutic potential of renin-angiotensin system inhibitors (RASi) in renal cell carcinoma (RCC) remains controversial. This meta-analysis synthe The renin-angiotensin-aldosterone system (RAAS) is central to the control of blood pressure and the target of several types of anti-hypertensive drugs. This pathway depicts a simplified representation of the pharmacodynamics (PD) of RAAS-acting drugs including candidate genes for the pharmacogenomics (PGx) of ACE inhibitors, angiotensin receptor blockers (ARBs), Efficacy outcomes were similar between groups (ACE inhibitor versus ARB, ACE inhibitor versus combination, ARB versus combination) as were rates of serious adverse events. The rate of permanent discontinuation for ARB monotherapy (6.3%) was significantly lower than for ACE inhibitor monotherapy (15.7%) or combined therapy (18.3%).
Direct renin inhibitors, a new class of antihypertensive drugs, block the RAS pathway at the point of activation. Inhibition of renin prevents the downstream production of the potent vasoconstrictor angiotensin II, which is responsible for increasing blood pressure. Abstract Rationale & objective: It is unknown whether initiating renin-angiotensin system (RAS) inhibitor therapy in patients with advanced chronic kidney disease (CKD) is superior to alternative antihypertensive agents such as calcium channel blockers (CCBs). Renin-angiotensin system (RAS) inhibitors reduce risk of kidney failure in patients with chronic kidney disease, but worsen kidney function in heart failure patients, especially in those with chronic kidney disease. Less is known about risk of kidney failure in heart failure patients receiving RAS inhibitors.
Introduction: Heart failure (HF) is still a major cause of morbidity and mortality all over the world. Aim of the study was to assess the benefits and harms of sacubitril/valsartan (S/V) compared to angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB) in Chronic treatment of hypertension or heart failure very often includes an angiotensin-converting enzyme inhibitors (ACE-Is) or angiotensin receptor blockers (ARBs) as renin-angiotensin system inhibitors (RASi) treatments. To stop or not to stop these In hypertensive patients with diabetes, the effectiveness of renin-angiotensin system (RAS) inhibitors in improving mortality, cardiovascular events, and renal outcomes, compared to other
ACE Inhibitor Pathway, Pharmacodynamics
Abstract Renin-angiotensin-aldosterone system (RAAS) inhibitors, including angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), are commonly used in the management of hypertension. High blood pressure is a vital risk factor for cardiovascular disease. This study aims to establish any significant difference in using ACEIs First-line drugs inhibiting the renin angiotensin system versus other first-line antihypertensive drug classes for hypertension. Cochrane Database of Systematic Reviews 2018, Issue 11.
Renin inhibitors are antihypertensive drugs which block the first step in the renin-angiotensin system. Their mechanism of action differs from that of angiotensin converting enzyme inhibitors and angiotensin receptor antagonists, but like these drugs, renin inhibitors interrupt the negative feedback effects of angiotensin II on renin
- Renolit Alkorplan F Bright Cool Roof Single Ply Roofing Membrane
- Report Excessive Dog Barking , Reducing barking: guidance for dog owners
- Replacing Lg Tv Remote | 6 Best Replacement Remotes for LG TV in 2025
- Remove The Header And Footer From A Single Page In Wordpress
- Rent Convertible Cars In Barcelona
- Replace Space Between Two Words With An Underscore In A Vector
- Remembering The Hauntingly Terrible 2000 Nba Draft Class
- Rent A Car In Bari , Drivalia Rent a Car in Bari, Italien
- Renato Zero Tour 2024 | Renato Zero Setlist at Palazzo dello Sport, Rome
- Reportage Mercedes Ml 250 Bluetec 204Ch
- Remote Calibration Service , Electrochemistry Jan21.indd