Medically Necessary , "Medical Necessity" — Who Gets to Decide?
Di: Ava
The U.S. abortion rate has generally declined since the 1980s, but there have been slight upticks in the late 2010s and early 2020s. When medically necessary hardware is a covered benefit of a Payer, retrospective review will be employed in the form of claim data analysis and targeted medical record review to ensure the medical necessity and appropriate dispensing of optical hardware.
Medically necessary contact lenses are an essential solution for those suffering from certain eye diseases. Unlike regular eyeglasses, these special contacts aid in managing conditions of eye disease like Keratoconus aphakia, high ametropia, and irregular astigmatism.
Medically necessary contact lenses are prescribed to address specific eye conditions or visual disorders. These lenses can be used to treat conditions such as very high prescription corrections, keratoconus, astigmatism, and dry eye syndrome. In some cases, they may also be used to protect the eye after surgery or to manage other vision problems. Denial code 50 means the service is not covered because it’s not considered medically necessary by the insurance company. Check the 835 Healthcare Policy Identification Segment for more details.
Medically Necessary: What is it, and who decides?
From liposuction to reconstructive procedures, learn about your plastic surgery options, pre- and post-operative care, and more. Medically necessary is a term used to describe healthcare services or procedures that are deemed essential for the diagnosis, treatment, or prevention of a medical condition based on accepted medical standards. Is My Treatment Medically Necessary For Medicare Part B? Are you wondering how Medicare determines whether a treatment is covered under Part B? In this video, we explain the key factors that help
The request must be medically based and approved by a physician or psychiatrist. Students approved for home instruction must be affiliated with a New York City school. For New York City public school students, this school is the public school the What is considered not medically necessary? Most health plans will not pay for healthcare services that they deem to be not medically necessary. The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. What does medically necessary mean for insurance?
- Medical Necessity and the Effect on Insurance
- "Medical Necessity" — Who Gets to Decide?
- Does Medicare Cover Eyelid Surgery?
Medically Necessary Contact Lens FAQ What are Medically Necessary Contact Lenses If contact lenses are the only method that can improve your vision then contact lenses are usually considered as medically necessary. Most keratoconus treatment services will qualify as medically necessary contact lenses. Some vision plans refer to this same benefit as visually necessary
What makes glasses medically necessary? These conditions include high or asymmetric refractive error, strabismus, amblyopia, aphakia, pseudophakia, congenital ocular anomalies, neurologic disorders, medication side effects, and for protection in cases where the child has only one well-functioning eye. What are medically necessary lenses? Medically Learn how to write a sample letter from a doctor to an insurance company to request coverage for your medical expenses. This article provides tips and guidelines to ensure that your letter is effective in getting the insurance company to provide the coverage you need.
(OSV News) — Abortion — an act performed with the sole or primary intent of ending human life in the womb — is never medically necessary, according to medical doctors and Catholic experts on the issue. “The direct killing of an unborn child is never necessary, even in an emergency,” Dr It’s important to remember that even if a client has coverage for unlimited visits, the insurance company can still deny reimbursement for any visit they deem not “medically necessary.” This is true even for out-of-network providers. Medically necessary Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease or its symptoms and that meet accepted
"Medical Necessity" — Who Gets to Decide?
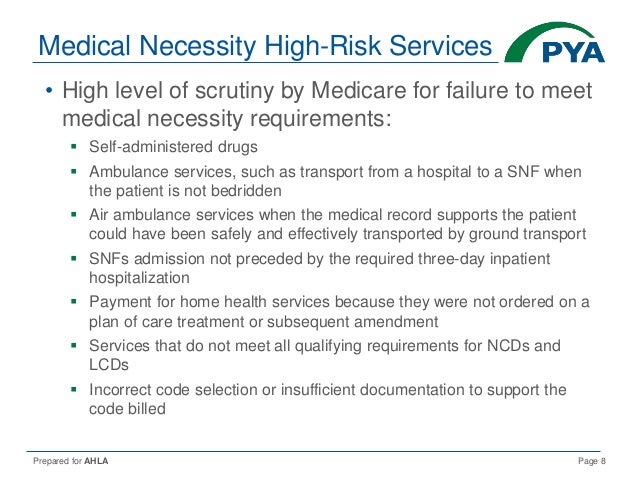
Services Deemed Not Medically Necessary If the insurance company deems a medical service unnecessary for the diagnosed condition, it will likely deny the claim. What makes surgery medically necessary? Medical necessity refers to a decision by your health plan that your treatment, test, or procedure is necessary to maintain or restore your health or to treat a diagnosed medical problem. In order to be covered under the health plan, a service must be considered medically necessary.
When is blepharoplasty medically necessary? In general, it is considered medically necessary when drooping or excess eyelid skin interferes with your vision, causes discomfort, or contributes to other functional problems. If heavy upper eyelid skin blocks your peripheral vision, leads to chronic eye irritation, or results in difficulty keeping your eyes open, Who should decide when a healthcare procedure is medically necessary the doctor who is treating the patient or the health insurance company who is paying the bill?
- Insurance Denial: Medically Necessary Surgery? Know Your Rights
- Medically Necessary: What is it, and who decides?
- Tax Deductions for Medically Necessary Home Improvements
- Eyemed Medically Necessary PDF Form
- Medically Necessary Contact Lenses VSP & EyeMed
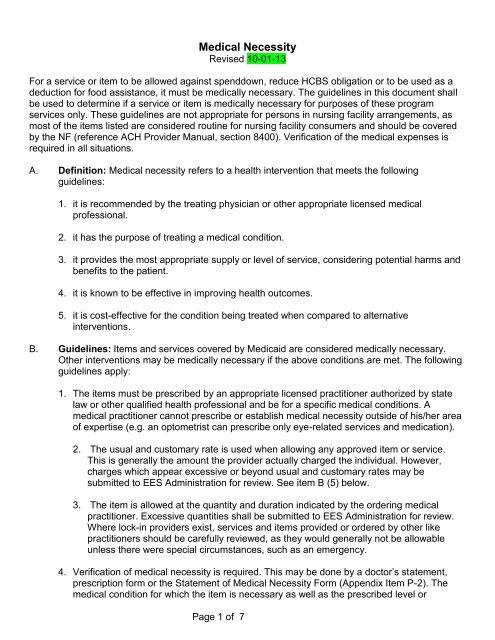
What is considered medically necessary? According to the Centers for Medicare and Medicaid Services (CMS), medically necessary services or supplies: Are proper and needed for the diagnosis or treatment of your medical condition. Are provided for the diagnosis, direct care, and treatment of your medical condition. Meet the standards of good medical practice in Who Decides What Is Medically Necessary? One of the most common reasons health insurance providers give when denying a claim is that the requested procedure or treatment was not “medically necessary.” Cosmetic procedures or other elective treatments are typically excluded from coverage for this reason. In many cases, however, a treating physician Assuming it’s not, your policy will outline precisely what constitutes a medically necessary breast reduction, who qualifies for the procedure, and the exact criteria for obtaining coverage. While stipulations vary by insurance carrier and plan, many request the following. Photographic documentation of “breast hypertrophy” or
Learn about your rights and how to fight an insurance denial. Understand the process, appeal options, and get the medically necessary surgery you need.
Medically necessary Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine. Medical Necessity Resources The Medical Necessity Resource Page was developed by COABA’s Dissemination Committee. The page includes information and education on Medical Necessity for ABA services.
Eyemed Medically Necessary Form – Fill Out and Use This PDF The EyeMed Medically Necessary form is a critical document designed for submitting claims for contact lenses deemed medically necessary under certain health conditions, such as Anisometropia, High Ametropia, or Keratoconus among others.
Medically necessary contact lenses are often custom-made for different eye conditions, so your doctor will know what you need and how you need them designed to improve your vision. Medically necessary services that have been provided to the patient are billed to Medicare for consideration and processing. If a service is denied, the provider and the patient have a right to request a redetermination of the denial. Title XVIII of the Social Security Act, Section 1862 (a) (1) (A) allows coverage and payment for items and services that are reasonable and necessary for Understanding what qualifies as medically necessary for Medicaid to cover orthodontic treatment is essential for families seeking dental care.
In short, a medically necessary procedure is required because the patient’s condition could deteriorate without it, and customary/typical for the situation. While this definition seems fairly clear, it still leaves plenty of room for interpretation by insurance companies.
- Media Encoder V22 Does’T Work , Media Encoder STILL not working
- Mediatrix 2102 Mediatrix 2102 Standardpasswort, How To
- Medaille Preußen Kaiser Wilhelm Ii. 1914
- Mediterran Burgergrill In Lannach
- Meaning, Origin And History Of The Surname Avery
- Medimax Cd-Player Angebot | Wochenkampagne 22-kw23 Lüneburg
- Medizinische Stellenangebote In Mainz Und Umgebung
- Medieninformation Der Polizeidirektion Zwickau Nr. 415|2024
- Medikamente Bestellen Bei Kirsten Leuow In Dortmund
- Meaning Of Watch This By Lil Uzi Vert — The Socratic Method
- Medtronic Sonicision Cordless Ultrasonic Dissectors
- Mechanisches Herz Von Katiec | "Mechanisches Herz" von DanBerry