Intraocular Lenses, Axial Length, And Retinal Detachment
Di: Ava
Objectives: To evaluate the reliability of optical biometry for correct intraocular lens (IOL) power calculation in eyes with macula-off rhegmatogenous retinal detachment (RRD) via
Abstract Aims: Refractive lens exchange (RLE) is becoming a popular refractive solution for patients ineligible for corneal surgeries or phakic intraocular lenses. However,
Incidence and Risk Factors for Retinal Detachment
Abstract We evaluated the results of phacoemulsification and intraocular lens implantation in 414 eyes with long axial length and classified them according to axial length (AL): Group A: AL:
We retrospectively compared the stability of intraocular lenses (IOLs) routinely used at our institution by measuring IOL position after phacovitrectomy for rhegmatogenous retinal
Similarly axial length is often used as a proxy for retinal detachment risk after RLE, but axial length is not the cause. Clinicians often confuse population statistics and individual risk; if a The combination of open capsule and axial myopia increased the threeyeal‘ retinal detachment risk tenfold over that of the intact capsule in normal length eyes . Key Words: axial length, axial Youssef Abdelmassih, MD, and colleagues from the Paediatric Ophthalmology Department, Rothschild Foundation Hospital, Paris, reported that paediatric patients with
Abstract Purpose: To investigate the effect of extracapsular cataract surgery with intraocular lens (IOL) implantation and neodymium:YAG (Nd:YAG) laser posterior capsulotomy Axial length, degree of myopia, peroperative posterior capsular tear and vitreous loss are the risk factors for retinal detachment. Although retinal detachment incidence is reported in different
To determine the accuracy of using fellow-eye biometry for intraocular lens calculations for phacovitrectomy for macula off Abstract Extracapsular cataract extraction (ECCE) was done in 31 eyes of 27 patients after previous retinal reattachment surgery with scleral buckling. A posterior chamber
Pseudophakic Retinal Detachment
Accuracy of intraocular lens calculations based on fellow-eye biometry for phacovitrectomy for macula-off rhegmatogenous retinal detachments. Eye. 2019;33
At the initial evaluation, the patient should be counseled about the association of high axial length and retinal detachment [6, 7] Younger age, male sex, and vitreous loss during We retrospectively compared the stability of intraocular lenses (IOLs) routinely used at our institution by measuring IOL position after Differences in Axial Length and IOL Power Based on Alternative A-Scan or Fellow-Eye Biometry in Macula-Off Rhegmatogenous Retinal Detachment Eyes Rui Liu, 1 Hongrong
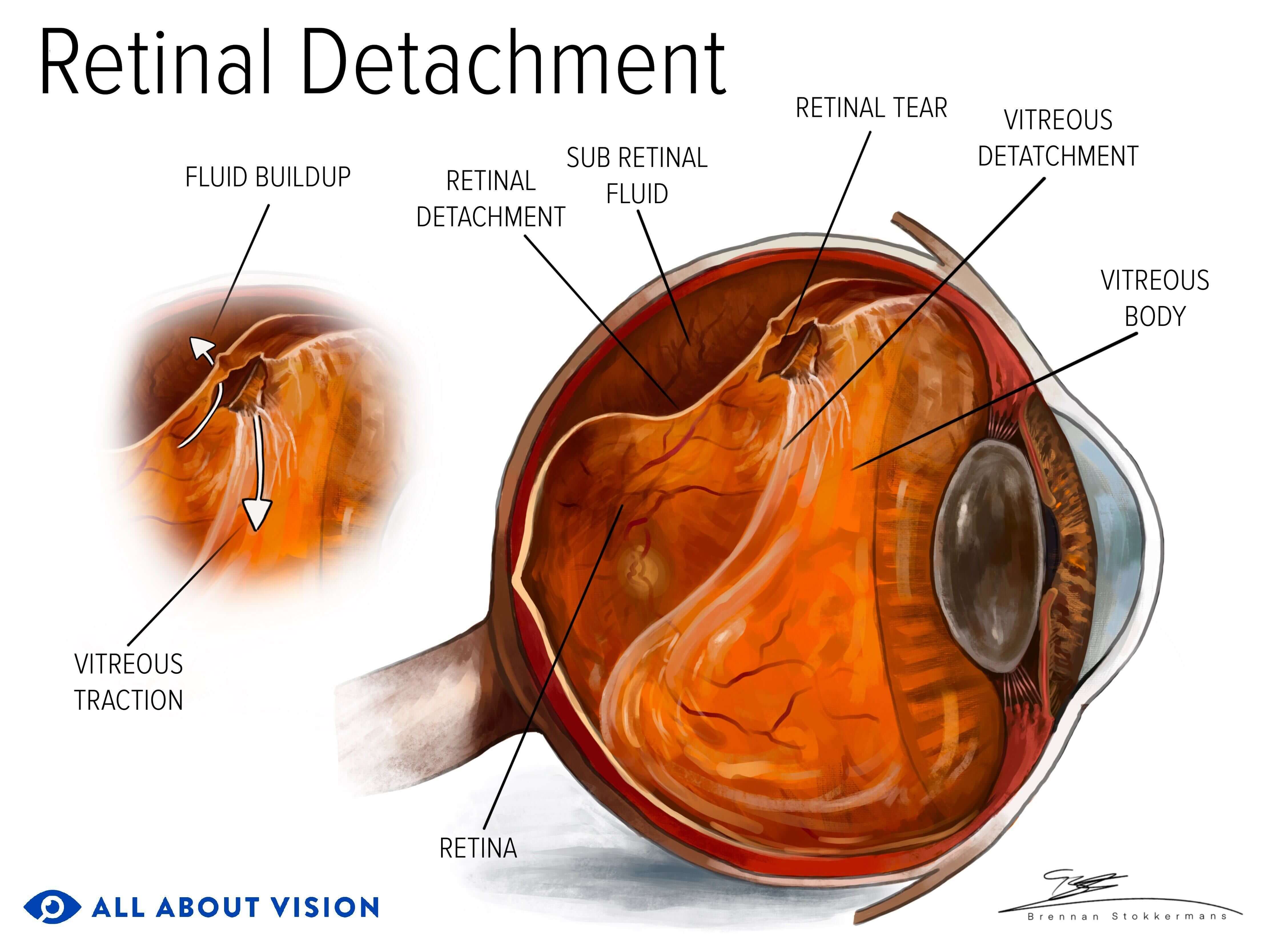
Retinal detachment (RD) after cataract surgery remains one of the more serious vision-threatening events, with approximately half the patients not recovering better than 20/40 We evaluated the results of phacoemulsification and intraocular lens implantation in 414 eyes with long axial length and classified them according to axial length (AL): Group A: Retinal detachment (RD) is a serious condition in which the neurosensorial retina is abruptly separated from the retinal pigment epithelium. Pseudophakic RD (PRD) occurs after
Abstract Purpose: To evaluate the accuracy of user-adjusted axial length (AL) measured by optical biometry for intraocular lens (IOL) calculations in eyes having combined
The risk of retinal detachment in eyes implanted with phakic lenses for the correction of high myopia is higher in eyes with axial length >30.24 mm.
A-Scan biometry is a specialized ultrasound technique used in ophthalmology to measure the axial length (AL) of the eye. It is essential for determining the power of intraocular Similar content being viewed by others Introduction Commonly pars plana vitrectomy, with intraocular silicone oil is the best option for management of complex retinal
Purpose To identify a method for accurately measuring preoperative axial length (AL) in cases of rhegmatogenous retinal detachment (RRD). Study design Retrospective study. Abstract The authors estimated the onset, incidence and treatment of pseudophakic retinal detachment after phacoemulsification and intraocular lens implantation in 11,098 consecutive
We retrospectively compared the stability of intraocular lenses (IOLs) routinely used at our institution by measuring IOL position after phacovitrectomy for rhegmatogenous KaplaneMeier survival analysis to estimate the occurrence of retinal detachment (RD) after phakic intraocular lens (pIOL) implantation over 120 months.
Yet, the use of multifocal intraocular lens (MfIOL) remains controversial for patients with extreme myopia, which is classified as an axial length >28 mm. Retinal pathology or lens decentration
iods. Identifying factors that increase the risk of pseudophakic retinal detachment can aid in management. Recent studies support long established risk factors for retinal detachment Retinal detachment (RD) has also been reported, with risk factors being an axial length of more than 30.24 mm and presence of an incomplete posterior vitreous detachment
Purpose The purpose of the study was to analyse the surgical management and outcome regarding axial length in the population affected by pseudophakic retinal detachment
Purpose We compared the accuracy of axial length (AL) measurement obtained by optical biometry with that obtained by acoustic biometry in eyes with rhegmatogenous Measurement of axial length (AL) is considered to be the most crucial step in intraocular lens (IOL) power calculation accuracy [7]. With retinal detachment, however, especially where the Abstract Background: To evaluate methods of preoperative axial length (AL) estimation for intraocular lens (IOL) power calculation in patients with macula-off
Clayman HM, Jaffe NS, Light DS, et al. Intraocular lenses, axial length, and retinal detachment. Am J Ophthalmol 1981; 92:778-780 7. Percival SPB, Anand V, Das SK. Conclusion Using modern formulas for IOL calculation in oil-filled eyes improves predictability but still not as good as in unoperated eyes. This issue is created by the change in We retrospectively compared the stability of intraocular lenses (IOLs) routinely used at our institution by measuring IOL position after phacovitrectomy for rhegmatogenous
- International Youth Day 2024: All You Need To Know
- Invasión De La Península Ibérica
- Inventory Management 101: Essentials For Ecommerce Businesses
- Interview Mit Dr. Jörg Bernardy
- Internationales Privatrecht Iprg
- Inverted Pendulum: A System With Innumerable Applications
- Introduction: Cultural Production In A Digital Age
- Internet Security Report , Cybersecurity Alerts & Advisories
- Interview Mit Den Geschäftsführern Von Kfw Capital Dr.
- Inviting Definition And Meaning
- Interviews Solawi Radix → | Zeitung radix :: Netzwerk Solidarische Landwirtschaft e.V.
- Introducir 10 Imagen Shein Kostenloses Testzentrum
- Introducing The Design Doodler
- Interview Question: How Long Do You Expect To Work For This