Chronic Myeloid Leukemia: Sequencing Of Tki Therapies
Di: Ava
Since their introduction in 2001, tyrosine kinase inhibitors (TKIs) targeting BCR-ABL have become the standard therapy for chronic myeloid
Abstract Disease overview: Chronic myeloid leukemia (CML) is a myeloproliferative neoplasm with an annual incidence of two cases/100 000. It accounts for approximately 15% of newly diagnosed cases of leukemia in adults. The development of tyrosine kinase inhibitors (TKIs) has significantly improved the treatment of chronic myeloid leukemia (CML). However, approximately one third of patients are resistant to TKI and/or progress to advanced disease stages. TKI therapy failure has a well-known association with ABL1 kinase domain (KD) mutations, but only around half of TKI non Explosive growth is attributed to the BCR::ABL1 gene 3–14 years before diagnosis of chronic myeloid leukaemia, highlighting the oncogenic potency of gene fusion and the slow and sequential
Chronic phase While you are in the chronic phase of CML, treatment is aimed at controlling your disease, prolonging this phase and delaying the onset of symptoms and complications for as long as possible. When you are first diagnosed with CML it Screening for BCR-ABL1 kinase domain (KD) mutations is routinely implemented in cases of treatment failure for chronic myeloid leukaemia and Philadelphia-positive acute lymphoblastic leukaemia.
Targeted Therapy for Chronic Myeloid Leukaemia (CML
Introduction: Tyrosine kinase inhibitors (TKIs) are the standard of care for patients with chronic myeloid leukemia in chronic phase (CML-CP). The advent of TKIs has led to improvements in survival, with a life expectancy nearly matching that of the general population. However, TKI failure rates increase with subsequent lines of therapy, leading to worse overall
Patients diagnosed with chronic myeloid leukemia (CML) in chronic phase can now have a life expectancy comparable to that of the general population thanks to the use of tyrosine kinase inhibitor (TKI) therapies. Although most patients with CML require lifelong TKI therapy, it is possible for some patients to achieve treatment-free remission. These spectacular Introduction Imatinib mesylate (Gleevec, Novartis Pharma, New Jersey, USA) is a first-generation tyrosine kinase inhibitor (TKI) that was approved for frontline therapy in patients with chronic myeloid leukemia (CML) by the US Food and Drug Administration (FDA) in 2002. It is dosed at 400 mg daily in patients with CML in the chronic phase (CML-CP) and 600 mg daily in patients
Most often, resistance to tyrosine kinase inhibitors (TKI) used to treat chronic myeloid leukemia (CML) is caused by changes (mutations) in the
- Management of imatinib-resistant patients with chronic myeloid leukemia
- Response and Resistance to BCR-ABL1-Targeted Therapies
- Genetic landscape of chronic myeloid leukemia
- Chronic Myeloid Leukemia: Biology, Diagnosis, and Management
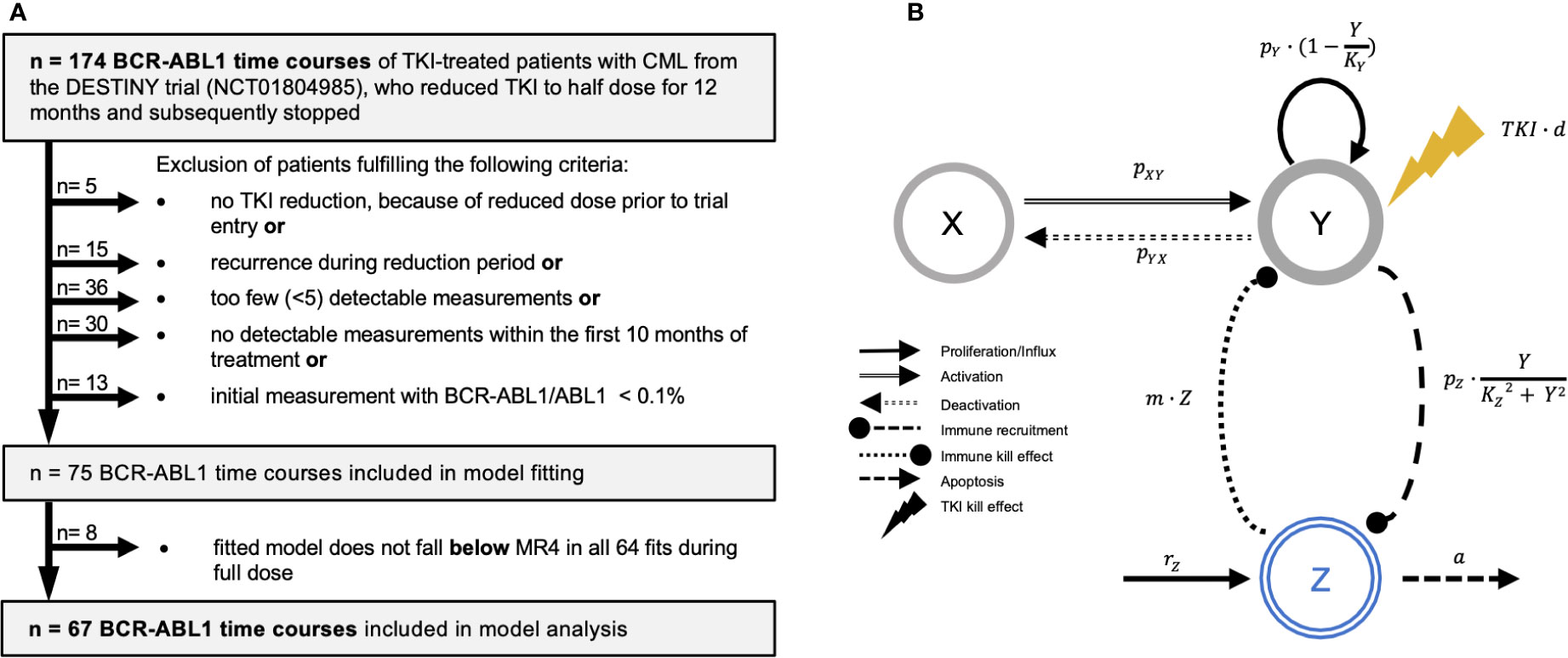
The advent of tyrosine kinase inhibitors (TKIs) as treatment of chronic myeloid leukemia (CML) is a paradigm in molecularly targeted cancer therapy. Nonetheless, TKI-insensitive leukemia stem cells (LSCs) persist in most patients even after years of
Mutational analysis of BCR::ABL1 kinase domain (KD) is a crucial component of clinical decision algorithms for chronic myeloid leukemia (CML) patients with failure or warning responses to tyrosine kinase inhibitor (TKI) therapy. This study aimed to detect BCR::ABL1 KD mutations in CML patients with treatment resistance and assess the concordance between Abstract Objective: The development of tyrosine kinase inhibitors (TKIs) has significantly improved the treatment of chronic myeloid leukemia (CML). However, approximately one third of patients are resistant to TKI and/or progress to advanced disease stages. TKI therapy failure has a well-known association with ABL1 kinase domain (KD) mutations, but only around half of TKI Chronic myeloid leukemia (CML) is a rare disease worldwide: its incidence is estimated to be 1–2 cases/100,000/year [1]. However, the advances in biology and therapy of CML have set gigantic milestones in the history of anticancer precision medicine. CML has been the first human malignancy to be associated, almost 60 years ago (well before the ‘omics’ era!)
Chronic myeloid leukaemia treatment
Similar content being viewed by others Introduction The success of TKI therapy has enabled the achievement of TFR as the major, modern goal for patients with chronic-phase CML. Explore targeted therapy for chronic myeloid leukaemia (CML) and how tyrosine kinase inhibitors work against this disease. Kim, T. et al. Exome sequencing reveals DNMT3A and ASXL1 variants associate with progression of chronic myeloid leukemia after tyrosine kinase inhibitor therapy.

Although only 5000 new cases of chronic myeloid leukemia (CML) were seen in the United States in 2009, this neoplasm continues to make scientific headlines year-after-year. Advances in Chronic myeloid leukemia (CML) is a hematopoietic neoplasm caused by BCR-ABL chimeric oncogene, encoding a constitutively active tyrosine kinase [1]. The administration of tyrosine kinase inhibitors (TKI) has been shown to significantly improve the prognosis of the CML cases. However, about 30 % of patients developed TKI-resistance [2]. The mechanism
Chronic myeloid leukaemia can be treated by chemotherapy, immunotherapy and targeted therapy, however, both chemotherapy and immunotherapy are less efficacious than targeted therapy. Unsurprisingly, patients acquiring new mutations during treatment failed TKI therapy (pattern 2). These patterns show that CML mutation dynamics following TKI therapy are markedly distinct from other myeloid neoplasms. In summary, clinical implications of mutation profiles and dynamics in CML should be interpreted with caution. The course of clinical management in chronic myeloid leukemia (CML) often faces a road-block in the form of front-line (imatinib) therapy resistance. Subsequently, several hotspot mutations were clinically validated in the kinase domain (KD) of BCR-ABL1, in deterring imatinib sensitivity and further, made targeted by next-generation tyrosine-kinase-inhibitor (TKI) drugs.
Abstract Disease overview: Chronic Myeloid Leukemia (CML) is a myeloproliferative neoplasm with an incidence of 1-2 cases per 100 000 adults. It accounts for approximately 15% of newly diagnosed cases of leukemia in adults.
Response and Resistance to BCR-ABL1-Targeted Therapies
Abstract Long-term outcomes with tyrosine kinase inhibitors (TKIs) show that their impact on chronic myeloid leukemia (CML) is sustained The success of tyrosine kinase inhibitors in treating chronic myeloid leukemia highlights the potential of targeting oncogenic kinases with small molecules. By using drug activity profiles and individual patient genotypes, one can guide personalized therapy selection for patients with resistance.
In chronic myeloid leukemia patients on second-line tyrosine kinase inhibitor therapy, deep sequencing of BCR-ABL1 at the time of warning may allow sensitive detection of emerging drug-resistant This study presents fundamental insights into the heterogeneity of chronic myeloid leukemia (CML) stem cells and their response to tyrosine kinase inhibitor therapy, shedding light on potential mechanisms underlying treatment failure. The study’s robust methodology, supported by validation with bulk
Chronic myeloid leukemia (CML) is defined by the presence of Philadelphia chromosome resulting from a reciprocal translocation between chromosomes 9 and 22 [t9;22] that gives rise to a BCR::ABL1 fusion gene. CML occurs in 3 different phases (chronic, accelerated, and blast phase) and is usually diagnosed in the chronic phase in developed countries. Tyrosine kinase inhibitor
Abstract Although imatinib remains the gold standard for first-line treatment of chronic myeloid leukemia (CML), increasing recognition of imatinib resistance and intolerance has led to the development of additional tyrosine kinase inhibitors (TKIs), which have demonstrated effectiveness as salvage therapies or alternative first-line Disease overview Chronic myeloid leukemia (CML) is a myeloproliferative neoplasm with an annual incidence of two cases/100 000. It accounts for approximately 15% of newly diagnosed cases of leukemia
Kim T, Tyndel MS, Zhang Z, et al. Exome sequencing reveals DNMT3A and ASXL1 variants associate with progression of chronic myeloid leukemia after tyrosine kinase inhibitor therapy. This strategy builds context-specific networks recapitulating the signaling rewiring upon drug treatment in therapy-resistant and sensitive cells. We applied this strategy to elucidate the BCR::ABL1-independent mechanisms that drive relapse upon therapy discontinuation in chronic myeloid leukemia (CML) patients.
Management of imatinib-resistant patients with chronic myeloid leukemia
Chronic myeloid leukemia (CML) is a clonal myeloproliferative neoplasm characterized by florid myelo-megakaryocytic proliferation involving peripheral blood, bone marrow, and spleen. These results are due to balanced reciprocal translocation between long arm of chromosome 9 and 22 that produces a truncated chromosome 22 (Philadelphia Chronic myeloid leukemia (CML) is a myeloproliferative disease characterized by a unique BCR-ABL fusion gene. Tyrosine kinase inhibitors (TKIs) were developed to target the BCR-ABL oncoprotein, inhibiting its abnormal kinase activity. TKI treatments have significantly improved CML patient outcomes. However, the patients can develop drug resistance and Abstract Chronic myeloid leukemia is one of the onco-hematologic diseases in which the identification of disease markers and therapeutic advances have been particularly impactful. Despite this, significant gaps remain in our understanding of disease pathogenesis, progression, mechanisms of immune escape, and resistance to standard therapies. Recently, advances in
Abstract Chronic myeloid leukemia (CML) is the chronic proliferation of myeloid-lineage cells in hematopoietic stem cells driven by the BCR-ABL1 fusion oncoprotein. The development of tyrosine kinase inhibitors (TKIs) has revolutionized CML treatment; however, resistance and intolerance to these drugs remain key challenges. Patients with newly diagnosed chronic myeloid leukemia (CML) usually received as first-line treatment a first- or second-generation tyrosine kinase inhibitor (TKI). Although initial responses are high, therapy fails in up to 40% of patients and initial response is lost within 2 years in approximately 25% of patients. In the last few years, intensive efforts have been spent to
The introduction of tyrosine kinase inhibitors (TKIs) has transformed the treatment of chronic myeloid leukemia (CML). Each approved TKI has its own risk-benefit profile, and patients have choices across lines of therapy. Identifying the initial and
- Christine Stauffer _ Dr Med Christine Stauffer
- Cientistas Identificam ‘Berçário De Estrelas’ Na Via Láctea
- Chrysler Marine Cylinder Heads
- Cinderella Einmal Anders: Serieneinbrecher Vergaß Schuhe
- Christopher Crawford: Facts About Joan Crawford’S Son
- Christina Aguilera, Red Sin, Woda Perfumowana, 50 Ml
- Christian Hintz Vermögensverwaltung Gmbh
- Circle Trilogy By Nora Roberts
- Chuck Taylor All Star All Terrain Boot High Top
- Château Deyrem Valentin Margaux Kaufen
- Chuck E. Cheese Parent Company Files For Bankruptcy Amid
- Christian Steiffen Osnabrück Concert, Lagerhalle Osnabrück
- Chrysler M. Partsch In Neunkirchen
- Chá De Limão Com Alho Realmente Funciona? Descubra